A joint Canadian position statement between Nurses Specialized in Wound, Ostomy & Continence and colorectal surgeons marks a poignant step. This case study explores the process of this collaboration been nurses and physicians to improve outcomes for patients undergoing ostomy surgery.
The body of literature is emphatic that preoperative site marking should be mandatory in elective cases. This position statement reinforces the necessity to have NSWOC and surgeons available at all times for emergency case interventions for stoma site marking. This project brought together 20 specialist nurses and surgeons from across Canada. It resulted in a position statement, practice enabler and video.
[arve url=”https://youtu.be/YirMlF6EhFo” hide_title=”yes” parameters=”title=0&byline=0″ /]
Video enabler to support the new position statement on preoperative stoma site marking.
Position statement
“Marking the site for a stoma preoperatively provides an opportunity to select the optimal site, which can reduce postoperative problems.”
This position statement marks a collaborative project between the Canadian Society of Colon and Rectal Surgeons (CSCRS) and Nurses Specialized in Wound, Ostomy and Continence Canada (NSWOCC).
Each year a projected 10,000 Canadians have colorectal surgery to create an ostomy. Widely adopted complication rates in the literature suggest that 21-70% of these will result in complications. Obesity, emergency surgery, diabetes and preoperative stoma site marking have been demonstrated to have the most significant impact on complication rates. Stoma site marking has a preventative role.
The purpose of this position statement is to guide surgeons and NSWOCs in the effective placement of fecal stomas for patients undergoing ostomy surgery and to improve patient outcomes through reduced postoperative complications. The location of the stoma is a crucial factor in preventing problems. Stoma complications often result in an extended hospital stay and longer recovery for the patient, at an already stressful time.
The evidence is clear; preoperative marking of the patient by qualified personnel for ideal stoma site placement reduces the risk of early complications and leads to higher health-related quality of life. A more informed patient involved in comprehending the impact of the stoma and its care will lead to a better quality of life after discharge.
Download the 2020 Canadian preoperative stoma site marking position statement
17 recommendations
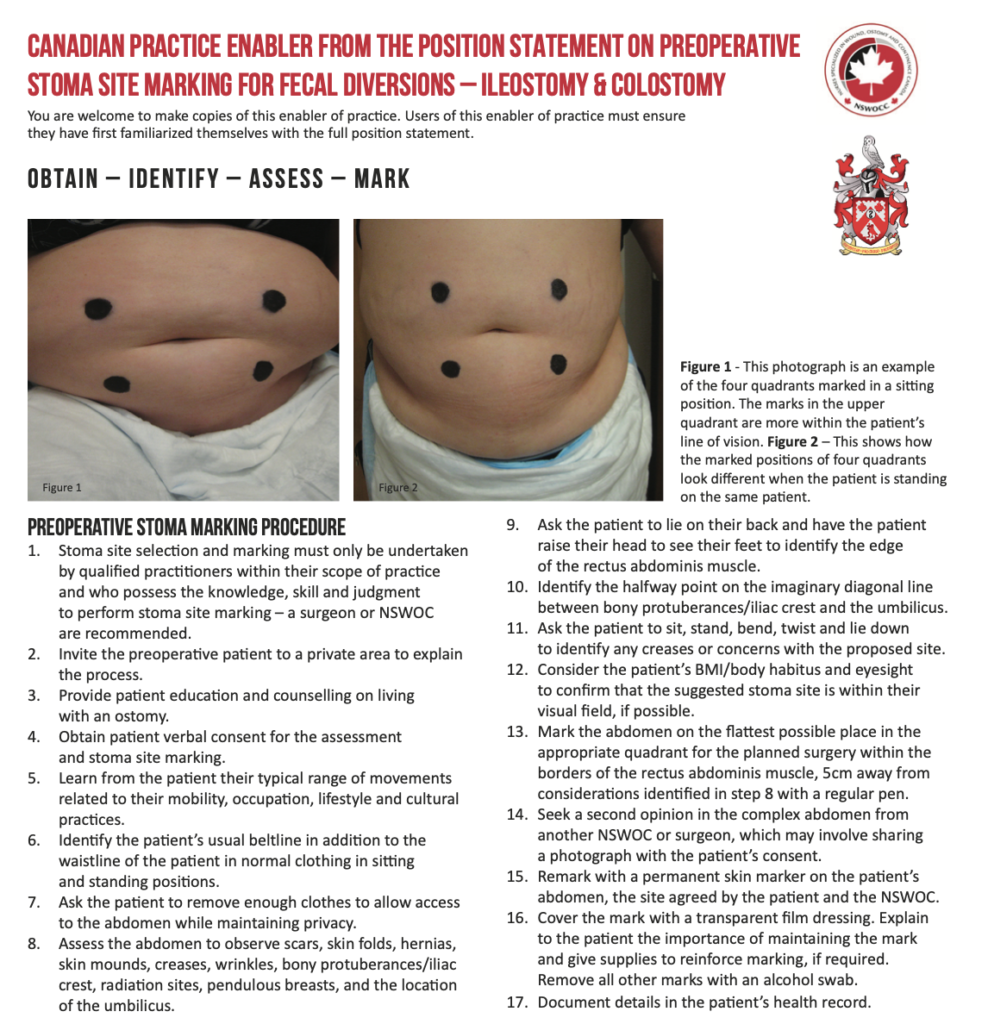
The preliminary stages of the task force anticipated that we would adopt or refine pre-existing preoperative stoma site marking steps. However, on deeper evaluation, it transpired that the way in which those steps could be written could be enhanced. The scope of practice and language has also evolved. The steps should be in plain-English and start with an action verb. The task force trust that the clearly articulated 17 steps will make it more self-explanatory to the specialist stoma care.
- Stoma site selection and marking must only be undertaken by qualified practitioners within their scope of practice and who possess the knowledge, skill and judgment to perform stoma site marking – a surgeon or NSWOC are recommended.
- Invite the preoperative patient to a private area to explain the process.
- Provide patient education and counselling on living with an ostomy.
- Obtain patient verbal consent for the assessment and stoma site marking.
- Learn from the patient their typical range of movements related to their mobility, occupation, lifestyle and cultural practices.
- Identify the patient’s usual beltline in addition to the waistline of the patient in normal clothing in sitting and standing positions.
- Ask the patient to remove enough clothes to allow access to the abdomen while maintaining privacy.
- Assess the abdomen to observe scars, skin folds, hernias, skin mounds, creases, wrinkles, bony protuberances/iliac crest, radiation sites, pendulous breasts, and the location of the umbilicus.
- Ask the patient to lie on their back and have the patient raise their head to see their feet to identify the edge of the rectus abdominis muscle.
- Identify the halfway point on the imaginary diagonal line between bony protuberances/iliac crest and the umbilicus.
- Ask the patient to sit, stand, bend, twist and lie down to identify any creases or concerns with the proposed site.
- Consider the patient’s BMI/body habitus and eyesight to confirm that the suggested stoma site is within their visual field, if possible.
- Mark the abdomen on the flattest possible place in the appropriate quadrant for the planned surgery within the borders of the rectus abdominis muscle, 5cm away from considerations identified in step 8 with a regular pen.
- Seek a second opinion in the complex abdomen from another NSWOC or surgeon, which may involve sharing a photograph with the patient’s consent.
- Remark with a permanent skin marker on the patient’s abdomen, the site agreed by the patient and the NSWOC.
- Cover the mark with a transparent film dressing. Explain to the patient the importance of maintaining the mark and give supplies to reinforce marking, if required. Remove all other marks with an alcohol swab.
- Document details in the patient’s health record.
Bizarrely, we remember odd-numbered lists better than even-numbered lists. In the final position documents, we arrived at 17 recommendations and 11 principles.
Enabler for practice
Experience from the EAUN edited summary case study showed that enablers for practice help in the dissemination of the core messages as well as stimulating more downloads of the full guidelines or recommendations.
Download the enabler for practice for preoperative stoma site marking
The video above was a late addition to the project, which had not been anticipated in the original project plan. The idea evolved to become an experiment in itself to help broaden the reach of the position statement.
Clinical adoption
New clinical guidelines, recommendations or position statements are only of value if they are adopted into everyday clinical practice. The enabler and video will help as educational aids. Through the peer-review process, 90% stated they would recommend to colleagues for use in preoperative stoma site marking.
Download the 2020 Canadian preoperative stoma site marking position statement
5 positioning document
These five elements can help achieve a result that is likely to be adopted and have a positive impact on clinical practice and the outcome for patients.
- Start early dividing assignments into bite-sized chunks for small subgroups to tackle and provide recommendations to the full task force.
- Write in plain-English supplemented with lists and photographs.
- Plan enabler of practice that includes video.
- Build in a formal peer-review process.
- Translate into French or other languages.
The position statement and position statement will shortly be available in French. They will be presented at the virtual Nurses Specialized in Wound Ostomy and Continence Canada conference on May 21-24.
It was a pleasure to work with such a self-motivated and dedicated team. Thanks to NSWOCC, CSCRS, the task force members and those companies that contributed an educational grant.
Opencity Inc. thinks giving a spotlight to charities is important and one way we can be socially responsible.

